Gm e-log
K Mahendra roll no 56 8th Sem
This elog depicts the patient centered approach to learning . This is an online E log book recorded to discuss and comprehend our patients de-identified health data shared , after taking his /her /guardians signed informed consent . This elog also reflects patients I centered learning portfolio.
55 year old male came to opd with chief complaints of fever and yellowish discoloration of eyes and tongue( jaundice) since 15days
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 15 days ago when he developed fever which was insidious in onset, low grade, gradually progressive in nature, associated with chills and rigors.
No hlo loose stools, vomitings
Pedal edema was noted by patient 2 days ago, pitting type
No h/o decreased urine output or burning micturation.
H/o cough since 1 day, non productive, dry cough.
No hlo chest pain, palpitations and sob
H/o yellowish discoloration of eyes and tongue since 15 days
No h/o bleeding per rectum, haematuria .
PAST HISTORY
K/c/o Diabetis mellitus II since 6 years, on unknown medication
N/k/c/o HTN, BA ,CVA , CAD , TB, Epilepsy
H/O Leprosy ? Hypopigmented patches ,7 months ago.
Medication one month ago?
No surgical history
H/o Blood transfusion , 5 days back. No reactions. Indications?
PERSONAL HISTORY
Married
Mixed diet
Decreased Appetite
Regular Bowel and bladder
No allergies
Alcoholic since 20 years, stopped one year ago.
FAMILY HISTORY
Not significant
GENERAL EXAMINATION:
Patient is conscious, coherent and co-operative,well oriented to time,place and person.
Moderately build and well nourished.
Examination was done in a well lit room.
Pedal edema + ( grade 2)
Icterus +
No pallor, cyanosis,clubbing,lymphadenopathy
Vitals
PR- 96 bpm
BP- 130/80 mm Hg
RR- 16 cpm
Temp -100 F
GRBS - 144 mg/dl
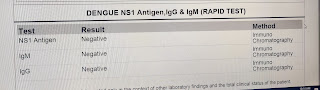
INVESTIGATIONS
31/10/23


































Comments
Post a Comment